Prevent Colorectal Cancer: Get Screened
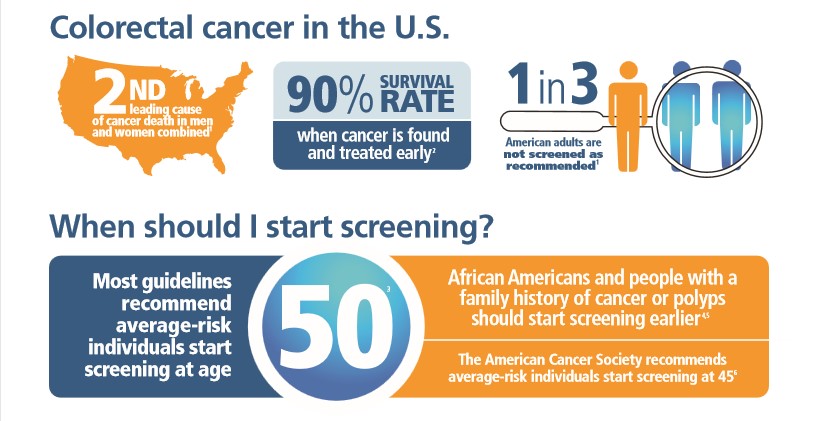
Colorectal cancer is the second leading cause of cancer death in the United States. It’s expected to kill more than 50,000 Americans this year alone. The good news? If caught early, the survival rate is very high.
That’s why screening for colorectal cancer is so important. Screening is generally recommended for all average-risk patients aged 50-75.
People who have a family member with colorectal cancer or polyps are at increased risk and might need to start screening before age 50.
High-risk factors include a personal history of polyps, inflammatory bowel disease, chronic ulcerative colitis, or a family history of colorectal cancer or polyps.
What are the Options for Screening?
There are four main ways to screen for colorectal cancer:
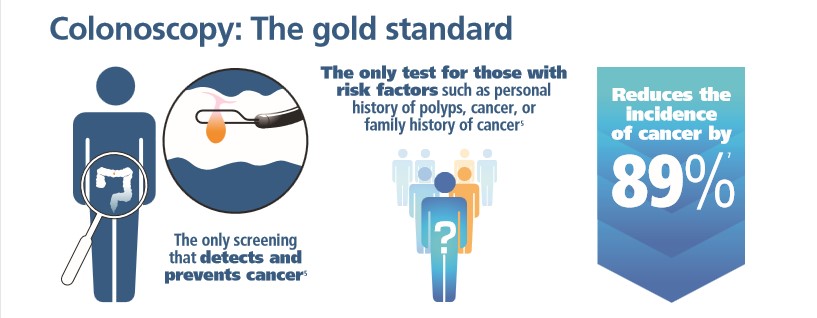
Colonoscopy: Colonoscopy uses a flexible, lighted tool called a colonoscope to view the entire colon and remove cancerous and precancerous growths called polyps if they are detected.
Fecal immunochemical test (FIT): This test checks the stool for tiny amounts of blood given off by polyps or colorectal cancer.
CT colonography: This involves a CT scanner and computer programs to create a three-dimensional view of the inside of the colon and rectum that can be used to identify polyps or cancer.
Cologuard: This tests the stool for tiny amounts of blood and identifies altered DNA from cancer or polyps that end up in the stool.
Which Screening Option is Best?
Preventing cancer should always be the first goal. Most colorectal cancers begin as polyps. Finding, quantifying, localizing, and removing polyps through screening colonoscopy is the most effective strategy for preventing colorectal cancer. That’s why colonoscopy remains the gold standard for colon cancer screening.
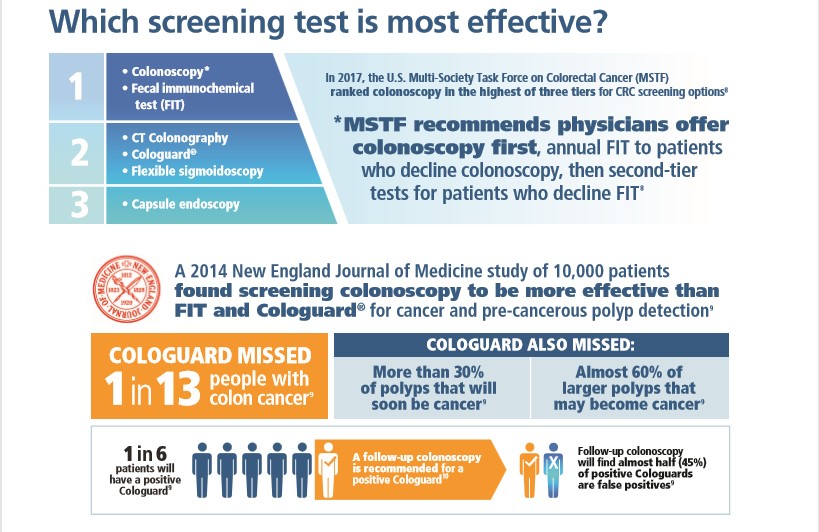
The Multi-Society Task Force on Colorectal Cancer recommends that physicians should offer colonoscopy first. For patients who decline to have a colonoscopy, the FIT test should be offered next, followed by second-tier tests such as Cologuard and CT colonography for patients who decline both first-line options.
A 2014 study published in the New England Journal of Medicine of 10,000 patients found that screening colonoscopy was better at finding cancer than both Cologuard and the FIT test. FIT and Cologuard were also not as good as colonoscopy at finding pre-cancerous polyps – and unlike colonoscopy, FIT and Cologuard can’t remove polyps.
Cologuard missed 1 in 13 people who had colorectal cancer detected by screening colonoscopy. Cologuard also missed more than 30 percent of polyps that will soon be cancer and almost 60 percent of polyps that may become cancer.
The FIT test missed almost 1 in 4 people who had colorectal cancer detected by screening colonoscopy. FIT also missed more than 50 percent of polyps that will soon be cancer and more than 75 percent of polyps that may become cancer.
Check with Your Insurance Provider
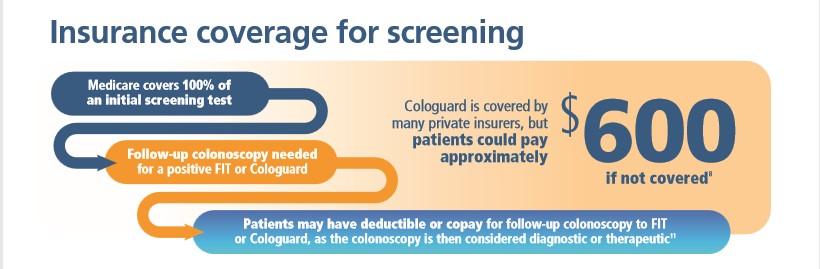
Patients may also have insurance considerations when choosing a test. A follow-up colonoscopy is recommended for positive FIT and Cologuard tests. Individuals with a positive FIT test or Cologuard test who are covered by Medicare may face a costly co-insurance bill after the recommended follow-up colonoscopy.
While insurance covers 100 percent of the preventive screening test, a follow-up colonoscopy for a positive FIT or Cologuard is considered a diagnostic or therapeutic service and may not be fully covered.
Almost one in six people who use the Cologuard test will have a positive result that suggests the presence of colorectal cancer. For almost half of those patients (45 percent), the colonoscopy will show their result from the Cologuard test was a false positive.
Check with your insurance provider before you are screened. Ask how much you should expect to pay if you need a follow-up colonoscopy for a positive FIT or Cologuard test result. This can help you avoid surprise costs.
Talk with Your Doctor
There are several ways to be screened. Remember, Colonoscopy is the gold standard, but if you’re unable to be screened by colonoscopy there are other appropriate options. Talk with your primary care physician about which screening test is best for you and do research about the available options to ensure you’re choosing the best test according to science.