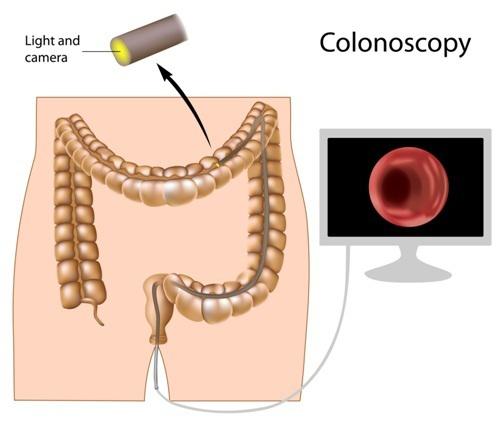
 Patients considering a colonoscopy in Louisville need to understand what happens during the procedure. A colonoscopy involves the use of a thin, flexible tube with a light source and camera to examine the lining of the large intestine (colon); the resulting images are displayed on a video monitor. This procedure is most commonly recommended as a screening test for colorectal, or colon, cancer. Colon cancer is the second leading cause of cancer-related deaths in the US today, with about 150,000 cases diagnosed annually. Colon cancer starts from polyps, which are abnormal growths to the colon lining. It takes years for polyps to grow into cancer, so if they are found during colonoscopy, they are then removed before cancer can develop.
Patients considering a colonoscopy in Louisville need to understand what happens during the procedure. A colonoscopy involves the use of a thin, flexible tube with a light source and camera to examine the lining of the large intestine (colon); the resulting images are displayed on a video monitor. This procedure is most commonly recommended as a screening test for colorectal, or colon, cancer. Colon cancer is the second leading cause of cancer-related deaths in the US today, with about 150,000 cases diagnosed annually. Colon cancer starts from polyps, which are abnormal growths to the colon lining. It takes years for polyps to grow into cancer, so if they are found during colonoscopy, they are then removed before cancer can develop.
An effective diagnostic tool, colonoscopy is also performed to evaluate patients for symptoms of bleeding, diarrhea and abdominal pain.
Please check out ValueOfColonoscopy.org for video/audio/presentation resources and patient tools on the importance of colorectal cancer prevention and different screening methods.
How Do You Prepare for Colonoscopy?
Before undergoing a colonoscopy in Louisville, your GHP physician will go over some pre-operative instructions that you will need to follow in the days before your procedure. Following these instructions is essential to limit surgery risks and provide the best results.
- Stop certain medications. Prior to surgery, your GHP physician and their staff will need to be made aware of all medications that you are taking, especially blood-thinning medications. These may include Coumadin (warfarin), Plavix (clopidogrel), Xarelto (rivaroxaban), Pradaxa (dabigatran), Eliquis (apixaban) and Lovenox (enoxaparin). Since the use of these medications increases the risk of excessive bleeding, they should be stopped prior to your procedure. If you are using insulin, the dosage or timing will also need to be adjusted the day of the procedure. Doctor-prescribed aspirin may be continued before your procedure. In addition, your physician asks that you provide him or his staff with a list of medications to which you are allergic.
- Use our cleansing routine the day before. your GHP physician’s office will prescribe a cleansing routine (or “prep”), which consists of a powerful liquid laxative that is to be taken the day before the procedure in order to prepare your bowels. This cleansing routine is the MOST IMPORTANT part of the procedure. Following directions and having a good cleanse can decrease the need for an early repeat colonoscopy. your GHP physician’s’ office will give you further instructions on following this cleansing routine and other details to follow on the day before the procedure. These instructions include following a clear liquid diet the day before the procedure, and drinking lots of liquids.
What Happens During a Colonoscopy?
Colonoscopy is performed as an outpatient procedure. When you check in, you will be escorted to the “pre-op” area where an IV will be placed and nurses will take your medical information. You will also meet with an anesthesiologist to discuss the sedation for the procedure.
You will then be taken to a procedure room and connected to monitors that will monitor your blood pressure, heart rate and blood oxygen levels throughout the course of the procedure. The procedure itself takes about 20-30 minutes to complete, and with you under sedation and therefore able to feel no discomfort. Since you will be completely sedated before the start of the procedure, you will not awaken until after the colonoscopy is completed. You will be placed on your left side so that the colonoscope can be inserted into the anus and advanced to the end of the colon (the cecum). (In rare cases (~1%), the scope cannot be advanced to the cecum and additional tests may be required.) The colon lining is also examined during the insertion process.
After the cecum is reached, your GHP physician slowly withdraws the colonoscope to examine the lining of the colon more thoroughly. Depending on what is seen, he may obtain a biopsy (a small piece of tissue) for analysis.
If there is bleeding, several different methods may be used. Instruments may be advanced into the colonoscope to help with bleeding. Medications can also be injected into an area. Cauterization (sealing off blood vessels with heat treatment) may also be administered by different probes. And sometimes, small temporary clips are used to control bleeding.
If polyps are found, they are removed with a variety of different instruments that all fit through the colonoscopy. Most commonly, they will be removed with “snare polypectomy,” which is a wire loop, or snare, used to grab the polyp and then remove it from the colon lining. With larger-sized polyps, electrical current will be used with polypectomy to prevent bleeding.
None of these above-described techniques cause discomfort.
What Should You Expect after the Procedure?
Following the procedure, you will go to the “post-op” area to recover from sedation; there you will also be monitored for any potential complications from the procedure and/or sedation.
Once you are fully recovered, your GHP physician will provide you with an explanation of the findings from your procedure, along with a copy of the procedure report, patient information handouts and follow-up instructions. He will give you a full preliminary report at this time; however, it may take several days for the final results of biopsies to return.
After having a colonoscopy, you may have some cramping or feel bloated because of the air introduced into the colon during the procedure. These symptoms will subside quickly upon passing gas.
Due to the effects of sedation, patients are instructed not to drive, operate machinery or make important decisions for the 24 hours following the procedure. You will need to arrange for someone to drive you home after surgery.
You will be able to eat after you leave the hospital, unless instructed otherwise. The nursing staff will review this and other important post-op instructions with you prior to discharge.
Possible Complications and Risks
One rare, though feared, complication of colonoscopy is perforation, or a tear in the lining of the intestine. The overall average risk for this complication is about one in 4,000 colonoscopies, though when it happens it may require surgery to repair.
Bleeding can occur at a biopsy site or small polypectomy site; this is a minor complication and will stop on its own or can be stopped during the exam. There is a small risk of excessive bleeding that requires hospitalization, and usually a repeat colonoscopy, to stop. This most commonly occurs after larger-sized polyp(s) is/are removed.
Uncommon risks from sedation used for the colonoscopy are: reactions to sedation medications, possible aspiration of stomach contents into lungs and complications from heart and lung diseases.
Although complications are rare, it is important to recognize them early. Contact Gastroenterology Health Partner’s office if you notice severe abdominal pain, fever and chills or excessive rectal bleeding.
All of these risks must be balanced against the potential benefits of the procedure and the risks of alternative approaches to the condition.
Disclaimer: This information is intended to provide general guidance and does not provide definitive medical advice. It is not a definitive basis for diagnosis or treatment in any particular case. This material does not cover all information and is not intended as a substitute for professional medical care. It is important that you consult your doctor regarding your specific condition, contraindications and potential complications.





