The Colonoscopy: A Historical Timeline
As we approach the end of this year’s Colorectal Cancer Awareness Month, let’s take a closer look at something near and dear to our hearts: the colonoscopy.
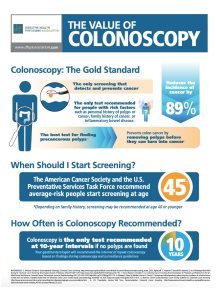
As the only screening test that detects and prevents cancer, the best test for finding precancerous polyps, and the only test recommended for people with risk factors such as personal history of polyps or cancer, the colonoscopy is truly a life-saving resource. Over 15 million colonoscopies are performed across the United States each year, reducing the widespread risk of colorectal cancer death by over 60%.
However, despite the colonoscopy’s widespread use and unequivocal standard of effectiveness, it is actually a fairly new methodology, one that took decades to be widely-known and well-established. While variations of the colonoscopy were first conceptualized throughout the 1960s, it wasn’t until the last few decades that the standards of quality which govern the colonoscopy as we know it came to be.
Follow along for a deep-dive into our favorite colorectal cancer screening test.
1960s-70s: The Early Years
Up until the mid-1960s, the closest thing to a colonoscopy was an endoscopic procedure using a rigid sigmoidoscope. This device had very limited movement, reach, and was unable to actually remove polyps.
In 1969, colleagues Dr. William Wolff and Dr. Hiromi Shinya of Beth Israel Medical Center in New York City invented the fiberoptic colonoscope, the first device to allow doctors to actually examine the entire length of the colon, thanks to its flexible, dynamic design.
Dr. Shinya also invented the polypectomy snare in 1969, a device which was able to physically remove colorectal polyps using a wire and electro-cauterizing mechanism.
By 1973, the pair had performed over 5,000 colonoscopies, demonstrating the validity and safety of the procedure.
1980s-90s: Increasing Awareness
In 1983, the Welch Allyn Corporation invented the first video endoscope, allowing doctors to see the procedure on-screen. Before, they were only able to observe the colon through a small eyepiece.
Although the colonoscopy continued to develop, there was still a lack of general public accessibility and awareness towards the procedure. Many people opted for tests such as fecal occult blood testing and sigmoidoscopy. It wasn’t until 1985, when President Ronald Reagan underwent a life-saving colonoscopy, that the procedure began to garner national attention.
In the mid-90s, the first screening recommendations were established in the United States. Adults over the age of 50 were suggested to receive regular colonoscopies. However, in a 1999 survey conducted by the CDC, only 40.3% of American adults over the age of 50 reported ever having a colonoscopy or sigmoidoscopy.
2000-Now: New Developments
In 2000, the American Society for Gastrointestinal Endoscopy (ASGE) published the first colonoscopy guidelines. This seminal work allowed the quality of a colonoscopy to be measured with a numeric value, the Adenoma Detection Rate (ADR) as well as evaluate measures such as the quality of bowel preparation, patient assessments, rate of complications, cecal intubation rate, and withdrawal time. Doctors were finally able to be pragmatically evaluated for their ability to perform a colonoscopy.
The early 21st century saw a significant increase in colonoscopies. Self-reported colonoscopies across the United States increased from 20% in 2000 to 47% in 2008. This can be contributed to many factors: a variety of educational campaigns and visibility measures pushed by doctors, government, and public organizations; Medicare coverage of colonoscopy, beginning in 2001; even celebrity stunts such as the Today Show’s Katie Couric’s publicized colonoscopy.
From 2000 to 2015, colon cancer rates rose considerably across increasingly younger populations. For adults aged 40-44, colorectal cancer incidence increased by 28%, for those aged 45-49, colorectal cancer increased by 15%, and while colonoscopy rates increased 17% in those aged 50–54.
Rising colorectal cancer rates have led to efforts such as the U.S. Preventive Services Task Force’s 2020 recommendation that all adults aged 45-75 should be regularly screened. This was an update from the 2016 guidelines that suggested adults without risk factors should begin screening at the age of 50.
What is the future of the colonoscopy?
The colonoscope of the present remains largely unchanged from that first created by Dr. Wolff and Shinya in 1969. While it has developed in mechanical quality, such as flexibility and control, and now features a light source, suction device, lens cleaning, and a camera, it doesn’t really vary in its fundamental use: to observe and remove colorectal polyps, acting as both a diagnostic and therapeutic instrument. Why is this the case? Likely because it is highly effective at what it does!
With this in mind, the most important development concerning colonoscopies, arguably, is in the public sphere. While the mechanisms of the procedure itself will undoubtedly continue to evolve and innovate, it’s important to consider the future of public access and opinion towards the colonoscopy.
There is still a surprising amount of misconception surrounding the colonoscopy. A 2020 survey of several European countries found that only 45% of people understood that it can prevent colon cancer. In the United States (pre-pandemic), around 68.8% of adults were up-to-date with their colonoscopy. Many people remain uninformed, fearful, and resistant to receiving the life-saving screening test. Other people are limited by financial means or geographic accessibility to the procedure.
By working to increase public awareness around the value of the colonoscopy, we can continue to prevent and reduce colorectal cancer deaths around the world. By educating your friends and loved ones about the importance of colonoscopy, partaking in events such as #DressInBlueDay and National Colorectal Cancer Awareness Month, getting involved with organizations like the Colon Cancer Coalition, and getting screened, yourself, you can help promote widespread change.
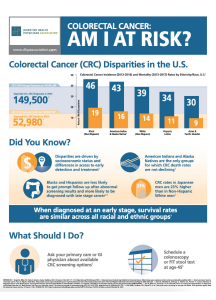
See new infographics created by the Digestive Health Physicians Association below. To read stories about people’s experiences with colonoscopies and colorectal cancer, click here. To see our favorite online resources for promoting awareness, click here. To learn more about what exactly colorectal cancer is, click here.