What is Colorectal Cancer?
Colorectal cancer refers to a cancer that starts in the colon or rectum. While cancers that start in either place may be called colon cancer or rectal cancer, respectively, they are often known collectively as colorectal cancer because of similarities between the cancers.
Here’s what you need to know about colorectal cancer.
Causes and Risk Factors
Scientists are not exactly sure what causes colorectal cancer. We do know that colorectal cancer begins when healthy cells’ DNA mutates. These cells can then overgrow and divide, creating tumors. Cancerous cells can also destroy healthy tissue and travel to other parts of the body and form deposits. However, there are several well-documented risk factors. These include being over 45, having diabetes, smoking, drinking alcohol, having a high-fat diet, having an inflammatory bowel disease, and having a family history of colon cancer or polyps.
Types
Most colorectal cancers (around 96%) are Adenocarcinomas. This kind of cancer starts in mucus-producing cells which lubricate the colon and rectum.
There are a few other kinds of colorectal cancers that are much more rare. Lymphomas, cancers of immune system cells, can start in the colon or rectum (although they typically start in lymph nodes). Carcinoid tumors start from hormone-producing cells in the intestine. Gastrointestinal stromal tumors start from cells in the colon wall, and while most are non-cancerous, some can be.
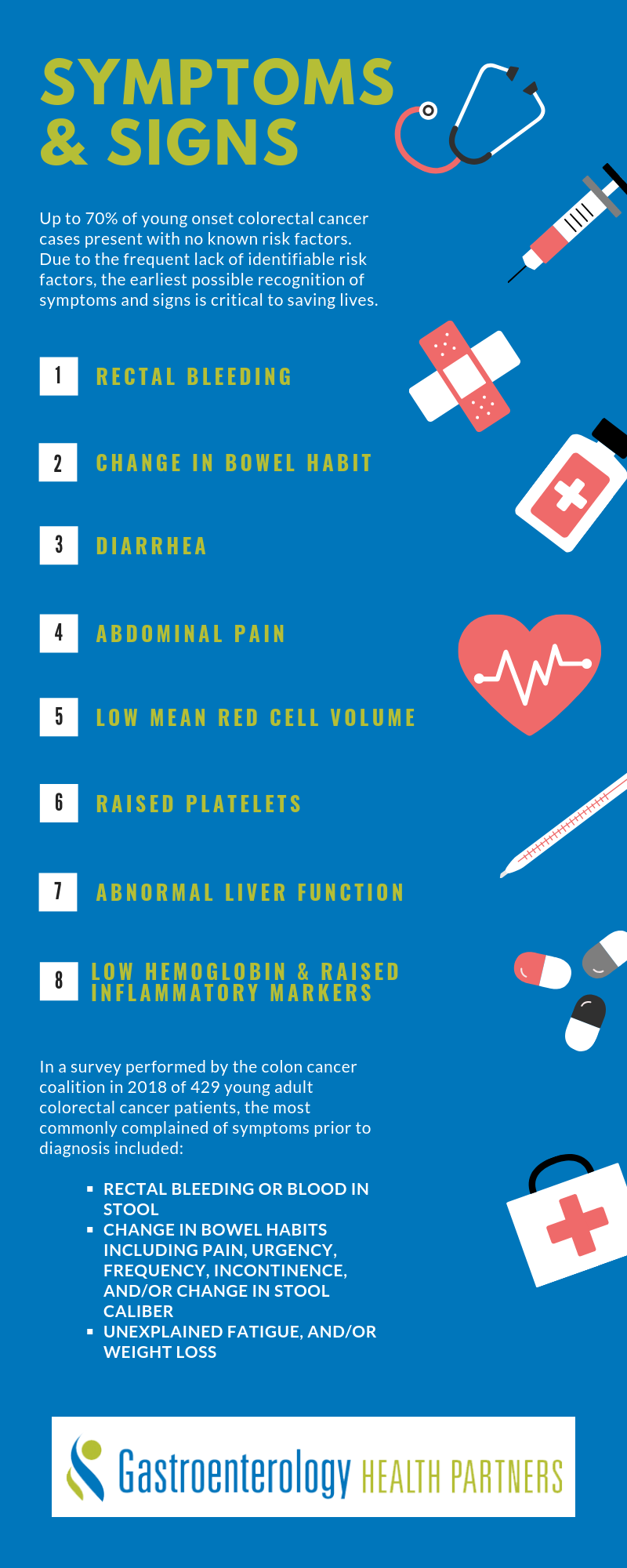
Symptoms
It’s common for colorectal cancers to have few symptoms until they have advanced. There are some potential warning signs, but they may be indicators of other issues. These symptoms include lower abdominal pain, blood in stool, bloating, cramps, vomiting, unexplained weight loss, and changes in bowel functions. As always, it’s best to consult a medical professional to determine what your symptoms are caused by.
Diagnosis
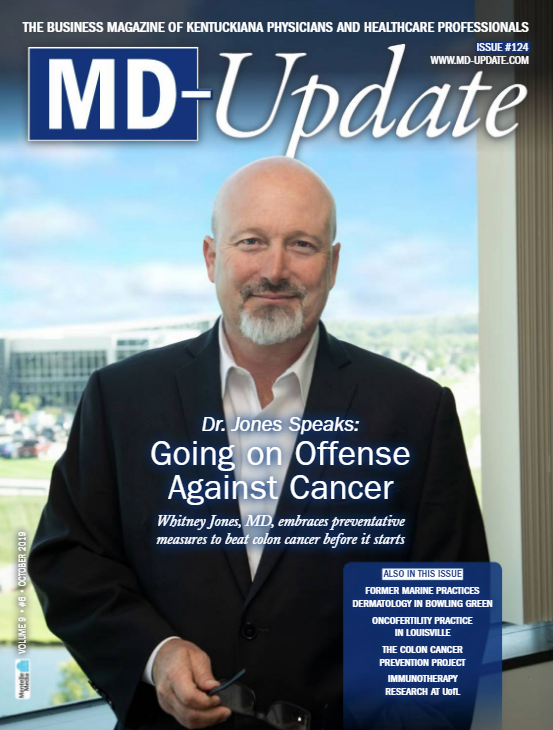
The best way to cure colon cancer is to identify it at an early stage. However, since symptoms may not present early on, doctors recommend screenings for healthy people, usually beginning around age 50. People with more risk factors, as discussed above, may be advised to be screened at a younger age.
A colonoscopy is one of the most common methods of screening. This involves using a scope to examine the inside of the colon. Your doctor can pass tools through the scope to take tissue samples if they see something suspicious. Biopsies of these tissue samples can help determine if cancer is present. Doctors also may remove polyps found during a colonoscopy to prevent them from becoming malignant.
Treatment and Prevention
There are three main treatments for colorectal cancer- surgery, chemotherapy, and radiation therapy. These three treatment options are often used together in various combinations, depending on a patient’s situation. The best treatment options for each person depends on factors including overall health, the cancer’s stage, and whether the cancer is recurring.
Localised, small, early-stage cancer in a polyp can be removed during a colonoscopy. A more invasive surgical procedure called a partial colectomy can remove the cancerous area of the colon and some surrounding healthy areas. This can prevent the cancer from growing back. Lymph nodes near the surgical site are removed and tested. Surgery can also be pursued to relieve symptoms and provide comfort for people in very poor conditions.
Chemotherapy is another treatment option, often used after surgery to destroy remaining cancer cells. If the cancer has spread beyond the colon lining, this may be recommended.
Radiation therapy utilizes beams of intense energy to destroy cancer cells. Radiation may be utilized before surgery to reduce tumor sizes, or after surgery to kill off remaining cancer cells.
Preventing colorectal cancer is extremely important, and it starts with screening (as discussed above). Additionally, you can reduce your risk of developing colorectal cancer by avoiding smoking, reducing or avoiding alcohol consumption, staying active, maintaining a healthy weight, and eating a healthy diet.
Our experienced team at GHP has years of experience helping people manage and treat colorectal cancer. We can help establish the best plan of care for your situation. Contact any of our office locations to learn about the options we offer and schedule an appointment today.